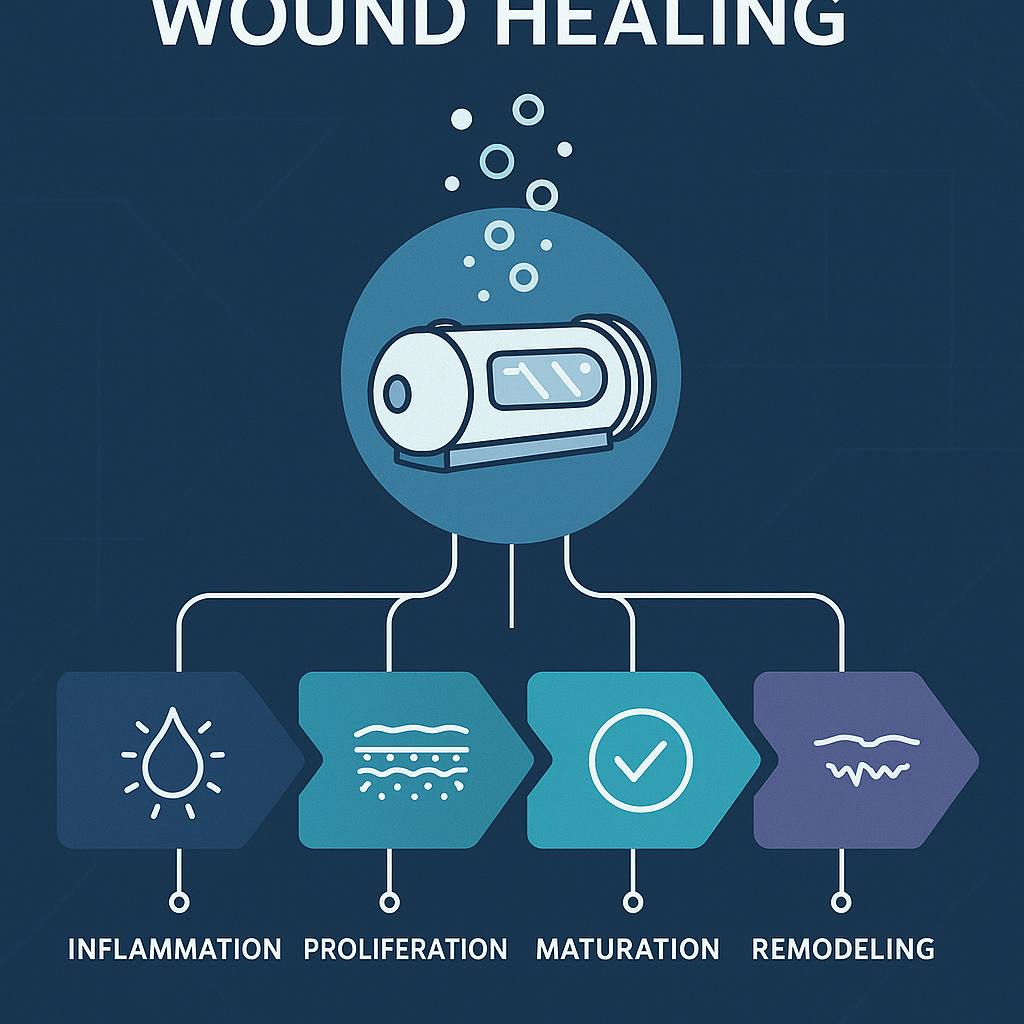
Phases of Wound Healing
The wound healing process is a complex and finely orchestrated sequence of events that can be broadly categorized into four distinct phases: hemostasis, inflammation, proliferation, and remodeling. Each of these phases relies heavily on oxygen as a critical factor to drive the biological processes necessary for effective tissue regeneration and healing.
- Hemostasis
Immediately after injury, this phase is activated to quickly stop bleeding through vessel constriction and platelet aggregation. Oxygen plays a crucial role here by supporting the energy requirements of platelets and facilitating the formation of a stable clot, which is critical for initiating the healing response. - Inflammation
Following hemostasis, there is an influx of immune cells such as neutrophils and macrophages to the wound site. Oxygen is pivotal for enabling the respiratory burst in neutrophils, a process essential for killing invading pathogens. Adequate oxygenation also enhances the bactericidal activities of immune cells, helping to prevent infection. - Proliferation
This phase focuses on rebuilding tissue structure, involving activities such as angiogenesis, collagen deposition, and re-epithelialization. Oxygen is indispensable for collagen synthesis by fibroblasts and promotes angiogenesis by acting as a signal for new blood vessel formation, ensuring sufficient blood supply and nutrients. - Remodeling
The final phase involves the reorganization and maturation of collagen fibers, strengthening the tissue structure. Oxygen facilitates the cross-linking of collagen, contributing to increased wound tensile strength. Sustained oxygen availability is critical to the efficient completion of the healing process and reducing the risk of wound dehiscence.
Hyperbaric oxygen therapy (HBOT) exploits this dependency on oxygen by providing higher concentrations to tissues, overcoming local hypoxia often associated with chronic wounds. For a detailed exploration of this therapeutic potential and its effects on wound healing, refer to the comprehensive review by Thackham et al., available here.
Effects of Hyperbaric Oxygen Therapy
Hyperbaric Oxygen Therapy (HBOT) significantly enhances the wound healing process through increased tissue oxygenation, which supports critical cellular functions. The efficacy of HBOT fundamentally lies in its capacity to deliver pure oxygen under elevated atmospheric pressures, raising the partial pressure of oxygen within tissues and facilitating accelerated healing processes.
- Enhanced Tissue Oxygenation
By delivering oxygen at higher levels, HBOT improves the energy availability crucial for cellular repair and replication processes, thus expediting the healing of ischemic tissues. - Reduction of Infection Risk
HBOT enhances the oxidative killing capabilities of leukocytes, such as neutrophils, which depend on oxygen for generating reactive oxygen species needed to destroy pathogens. Consequently, this therapy reduces wound infection risks, particularly in areas with compromised blood supply. - Promotion of Angiogenesis
HBOT stimulates angiogenesis by upregulating angiogenic growth factors and enhancing endothelial cell proliferation, thereby improving blood flow to the healing tissue. - Facilitation of Essential Cellular Activities
HBOT enhances fibroblast proliferation and collagen synthesis, key activities needed for reconstructing the dermal matrix. The therapy supports collagen maturation, which strengthens the structural integrity of healing tissues.
By incorporating HBOT into wound care regimens, the broader benefits encompass a comprehensive enhancement of the body’s natural healing processes, significantly improving clinical outcomes in challenging wound scenarios. More on these therapeutic mechanisms can be found in the review by Thackham et al., accessible here.
Mechanism of Hyperbaric Oxygen Therapy
Hyperbaric Oxygen Therapy (HBOT) employs physicochemical principles to foster enhanced wound healing—most notably in chronic conditions where conventional treatments have limited success. This therapy involves placing patients in hyperbaric chambers where they are exposed to pure oxygen at pressures significantly surpassing those found in the atmosphere.
The primary mechanism behind HBOT is the substantial increase in the partial pressure of oxygen in the bloodstream. At elevated pressures, oxygen dissolves in the plasma, allowing for greater tissue penetration compared to normobaric conditions. This hyperoxygenation alleviates local hypoxia commonly observed in chronic wounds.
- Angiogenesis Stimulation
Oxygen serves as a critical signaling molecule for angiogenic factors. By promoting new blood vessel formation, HBOT ensures restored circulation in the wound bed, thereby enhancing nutrient and oxygen supply. - Collagen Synthesis and Fibroblast Function
HBOT supports fibroblast activity and collagen synthesis, which are pivotal for new tissue structural integrity. Increased collagen deposition accelerates the reconstruction of the dermal matrix, crucial for wound closure. - Immune Modulation and Infection Control
The oxygen-rich environment bolsters leukocyte function, enhancing their bactericidal capabilities. Increased oxygen empowers neutrophils and macrophages to produce reactive oxygen species, thereby improving infection control in wounds.
HBOT presents a multi-faceted approach to overcoming the oxygen limitations present in wound beds and optimizing the physiological environment for healing. For an in-depth examination of these mechanisms in clinical practice, refer to Thackham et al.’s review here.
Protocol Standardization
Despite the promising benefits of Hyperbaric Oxygen Therapy (HBOT) in treating chronic wounds, the absence of standardized treatment protocols poses significant challenges to effective implementation. Standardized guidelines ideally outline the optimal pressure settings, treatment durations, and session frequencies required to achieve the best clinical outcomes.
- Pressure Parameters
Determining the optimal pressure critically influences the oxygen saturation in tissues. However, the current recommendations vary from 1.5 to 3 atmospheres, underscoring the need for empirical studies to establish pressures that maximize therapeutic efficacy while minimizing side effects. - Treatment Duration
While shorter durations may yield inadequate oxygen saturation, excessively lengthy sessions pose risks of oxygen toxicity. Balancing these considerations remains a challenge, typically based on clinician experience rather than robust supporting data. - Frequency of Sessions
The frequency of HBOT sessions widely varies, from daily treatments over several weeks to more spaced regimens. A clear consensus on the scheduling of sessions is necessary for both physiological outcomes and logistical feasibility. - Empirical Data Needs
The variable nature of wound etiologies and patient responsiveness calls for extensive clinical trials to produce empirical data that can inform personalized HBOT protocols. Such studies are essential for establishing evidence-based guidelines that optimize patient care.
Addressing these gaps is critical for broader acceptance and integration of HBOT into standardized wound care. Continued research should focus on multi-center trials to build comprehensive data sets that can facilitate optimal treatment regimens. More insights on these approaches are available in the review by Thackham et al., which can be accessed here.
Factors Influencing Wound Healing
While oxygen’s role in wound healing is paramount, multiple extrinsic and intrinsic factors significantly modulate the healing process. Effective management of these variables, alongside Hyperbaric Oxygen Therapy (HBOT), is essential for achieving optimal healing outcomes.
- Stress and Psychological Factors
Physiological stress can hinder healing, as cortisol disrupts normal repair processes. Addressing stress through management strategies is crucial for an optimal healing environment. - Nutritional Status
Deficiencies in essential nutrients like proteins, vitamins, and minerals can impede healing. Sufficient intake of nutrients such as vitamin C and zinc is necessary to support collagen formation and immune function, thereby enhancing HBOT efficacy. - Medications and Co-morbidities
Certain medications and chronic conditions like diabetes affect wound healing by impairing immune responses and microcirculation. Integrative management can optimize metabolic control, improve healing outcomes, and mitigate adverse medication effects. - Economic Justification vs. Medical Efficacy
The cost of HBOT raises questions regarding its economic feasibility in the healthcare system. The challenge lies in balancing financial commitments with the therapy’s long-term efficacy in reducing complications and costs for vulnerable populations.
A comprehensive understanding of these influencing factors is vital for refining HBOT protocols and ensuring patient access to effective treatment. For detailed insights on these aspects, consult the review by Thackham et al., available here.
Conclusion
The refinement of Hyperbaric Oxygen Therapy (HBOT) protocols stands as a crucial component in advancing wound management within regenerative medicine. As highlighted by Thackham et al., optimizing treatment parameters, including pressure, session duration, and frequency, is essential to maximize HBOT’s clinical benefits.
A shift towards robust theoretical models that incorporate individual patient variables—such as wound type and healing trajectories—will enable more personalized treatment plans. Integrating data science techniques, such as machine learning, can provide deeper insights into the multifactorial interactions affecting patient outcomes.
Additionally, empirical evidence supporting the long-term benefits and cost-effectiveness of HBOT is vital for its wider adoption. Comprehensive clinical trials will help validate and refine these treatment models, ensuring evidence-based practices lead to consistent, favorable outcomes for patients.
Advancing HBOT’s application necessitates a collaborative approach pooling expertise from various fields to enhance understanding and deployment of this therapy. In doing so, we can ensure HBOT remains integral to effective wound management, improving patient quality of life and addressing the burden of chronic wounds. For further insights into the ongoing developments in HBOT protocols, explore the review by Thackham et al. here.
Sources
- Wiley – The use of hyperbaric oxygen therapy to treat chronic wounds: a review (https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1524-475X.2008.00372.x)
- Thieme – Hyperbaric oxygen and wound healing (https://www.thieme-connect.com/products/ejournals/abstract/10.4103/0970-0358.101309)
- Wiley – Prognostic factors predicting ischemic wound healing following hyperbaric oxygenation therapy (https://onlinelibrary.wiley.com/doi/abs/10.1111/wrr.12038)
- UHMS – A clinical practice guideline for the use of hyperbaric oxygen therapy in the treatment of diabetic foot ulcers (https://www.uhms.org/images/CPG/UHM_42-3_CPG_for_DFU.pdf)
- Dove Press – Hyperbaric oxygen therapy for the management of chronic wounds: patient selection and perspectives (https://www.tandfonline.com/doi/abs/10.2147/CWCMR.S175721)
- LWW – An update on the appropriate role for hyperbaric oxygen: indications and evidence (https://journals.lww.com/plasreconsurg/fulltext/2016/09001/an_update_on_the_appropriate_role_for_hyperbaric.15.aspx)
- AIMSPress – Optimal switching time control of the hyperbaric oxygen therapy for a chronic wound (https://www.aimspress.com/fileOther/PDF/MBE/mbe-16-06-419.pdf)
- Springer – Oxygen in wound healing and infection (https://link.springer.com/article/10.1007/s00268-003-7398-5)