Synthetic polymers—tunable mechanics and degradation
Synthetic polymers such as Poly(lactic-co-glycolic acid) (PLGA) have revolutionized scaffold fabrication in tissue engineering due to their adjustable mechanical properties and degradation rates. By manipulating the lactic:glycolic acid ratio—50:50 for rapid hydrolysis or 85:15 for prolonged stability—engineers can align scaffold resorption with specific biological needs, such as bone or ligament regeneration. This versatility allows for compressive moduli within the range of 50–200 MPa, ensuring functionality during healing phases [Keane & Badylak, 2014].
Moreover, Polycaprolactone (PCL) boasts superior elongation properties (over 300%) and a slow degradation rate, often exceeding 24 months. This characteristic makes PCL particularly suitable for applications requiring mechanical integrity during the extended remodeling process. Techniques such as copolymerization and cooling rate optimization during electrospinning can yield fiber diameters down to 400 nm, enhancing osteoblast alignment and supporting cellular activities [Lee et al., 2014].
Natural polymers—biochemical cues for cell engagement
Natural polymers provide unique biochemical cues essential for enhancing cell adhesion and signaling. Collagen, for instance, inherently possesses RGD and GFOGER motifs that specifically bind to integrins α1β1 and α2β1, significantly promoting mesenchymal-stem-cell adhesion and osteogenic signaling. Research indicates that collagen gels maintain over 90% cell viability in vitro while upregulating alkaline phosphatase by two-fold compared to inert scaffolds like polyethylene [Parenteau-Bareil et al., 2010].
Alginate, another natural polymer, undergoes gentle Ca²⁺-mediated gelation, allowing for the encapsulation of sensitive cell types, such as chondrocytes or insulin-secreting islets, with minimal shear stress. Alginate beads, when ionically cross-linked, exhibit over 95% viability post-printing and can be chemically modified to tailor degradation rates, making them ideal for matching timelines in cartilage or wound healing [Christensen, 2011].
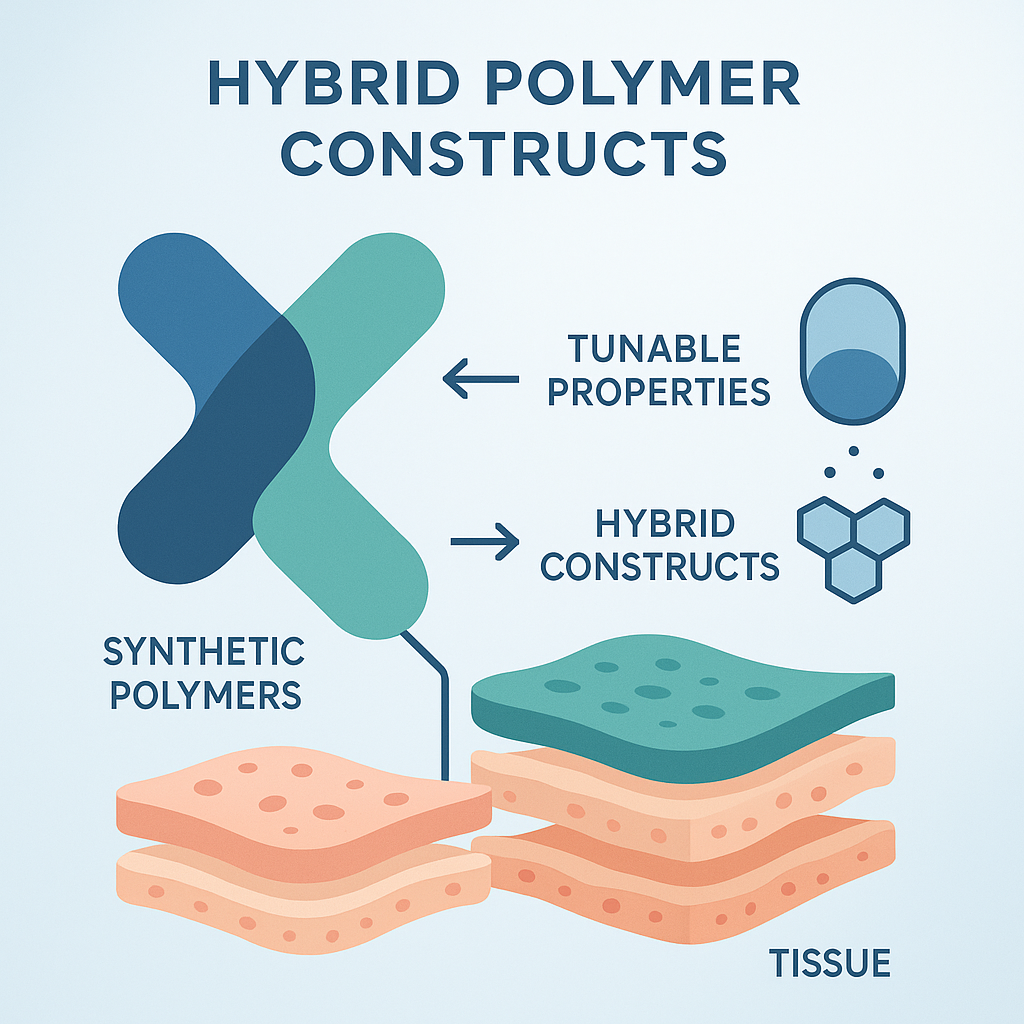
Hybrid constructs—merging strength with bioactivity
The integration of synthetic and natural polymers results in hybrid constructs that boast unique mechanical and biological properties. For instance, PLGA microfibers blended within a collagen-alginate matrix create composite hydrogels that mirror the compressive modulus (200–400 kPa) of native articular cartilage, while retaining the necessary bioactive elements that support chondrocyte phenotype maintenance [Hubbell, 1995]. This synergy highlights how synthetic materials contribute structural precision and mechanical stability, while natural polymers enhance bioactivity and cellular interactions.
Thermosensitive platforms
Thermosensitive biomaterials have transformed scaffold applications by enabling responsive behavior to physiological temperature changes. For example, injectable poly(N-isopropylacrylamide) (PNIPAAm)-based hydrogels maintain a liquid state at room temperature but transition to a gel at body temperature. This property allows for minimally invasive delivery into anatomical defects, providing scaffolding in situ [Khan & Tanaka 2017].
Hybrid systems integrating PNIPAAm with chitosan can co-load mesenchymal stem cells, transitioning from a soft network at initial placement to a stiffer structure that enhances early chondrogenic commitment while still permitting nutrient diffusion [Lee et al. 2014].
pH-responsive systems
Engineered pH-responsive systems are another critical innovation, particularly for delivering therapeutics in hypoxic conditions. For instance, polyanhydride-block-polypeptide micelles disassemble below pH 6.5, releasing angiogenic factors like VEGF in ischemic environments, thereby facilitating localized neovascularization [Hubbell 1995]. Additionally, alginate matrices modified for pH-sensitive degradation exhibit rapid breakdown in the lactic-acid-rich milieu of healing bone, synchronizing scaffold degradation with tissue infilling [Christensen 2011].
Integrated smart-release strategies
Employing integrated smart-release strategies maximizes therapeutic efficacy by using dual-trigger platforms. For example, PNIPAAm microgels embedded within PLGA matrices create a scaffold that gels upon temperature elevation, providing immediate support, while the gradual degradation of PLGA ensures sustained release of BMP-2 over 4–6 weeks. This approach has been shown to double the bone volume in preclinical models compared to bolus delivery methods [Keane & Badylak 2014].
Electrospun and particulate-based delivery systems
Electrospinning technology has enabled the development of drug-loaded nanofibers that act as bioactive micro-reactors. Co-electrospinning PLGA nanospheres loaded with BMP-2 within PCL microfibers achieves a core-shell structure for controlled growth factor release (estimated at ~0.8 µg day⁻¹ for four weeks), significantly enhancing new bone formation in rat models compared to single-dose applications [Lee et al., 2014].
In another approach, gelatin/collagen microspheres functionalized with heparin can sequester VEGF, releasing it in response to matrix-metalloproteinase activity, ultimately driving increased micro-vessel density in large bone grafts [Hubbell, 1995].
Multimodal delivery platforms
Layer-by-layer assembly structures offer a strategic means of integrating fast-releasing and slow-degrading elements. For example, co-printing polypeptide films with PLGA cores provides a biphasic kinetic release, delivering an initial chemotactic pulse followed by sustained angiogenic signals. This technique effectively replicates natural wound healing cascades [Kohane & Langer, 2008]. Integrated design considerations also employ computational modeling to predict release kinetics and scaffold resorption, allowing for customization based on anticipated patient-specific needs [Khan & Tanaka, 2017].
3D printing for anatomical fidelity
Micro-CT-driven 3D printing techniques enhance the precision of scaffolds tailored for individual patients. High-resolution data enables the reproduction of intricate bone structures with ±50 µm accuracy, while maintaining scaffold performance through the incorporation of 500 µm interconnecting pores, facilitating mesenchymal-stem-cell migration [Keane & Badylak 2014].
Additionally, patient-specific constructs—like ear and nose shapes made from PCL and collagen inks—exhibit less than 5% deviation from their native geometries post-sterilization and implantation [Lee et al. 2014].
4D printing for intra-operative and in vivo adaptation
Emerging 4D printing technologies capitalize on materials that can respond dynamically to physiological conditions. For example, shape memory polyurethane embedded in PCL scaffolds can expand upon heating, precisely conforming to the anatomical landscapes of craniofacial structures during surgical procedures, which eliminates the need for mechanical hardware [Khan & Tanaka 2017].
Hydration-responsive composites also reveal promising capacities, as alginate-cellulose structures can unfurl in moist environments, effectively filling irregular defects much better than static models [Christensen 2011].
Bone and cartilage
Tissue engineering for bone and cartilage requires tailored mechanical and biological materials. Mineral-filled PLGA/β-TCP composites are engineered to provide compressive strengths that are compatible with native bone, simultaneously degrading to promote osteogenesis [Keane & Badylak 2014]. Conversely, cartilage applications strive for viscoelastic properties; hybrid PCL-collagen mats guide chondrocyte alignment, effectively enhancing glycosaminoglycan (GAG) production [Lee et al. 2014].
Vascular integration remains a critical challenge in these applications; sequestering VEGF within collagen scaffolds has been shown to significantly enhance micro-vessel density in vivo, accelerating the overall vascularization process essential for successful tissue regeneration [Hubbell, 1995].
Cardiac and vascular constructs
Innovative biomaterials designed for cardiac and vascular applications include elastin-mimetic, electroconductive hydrogels that facilitate synchronous contraction of engineered myocardium and sustain mechanical strains above 15% without fatigue. Moreover, these hydrogels pre-seeded with endothelial progenitors can form viable, lumenized vessels due to the controlled release of stromal-derived factors [Christensen 2011].
For small diameter vascular grafts, bilayer constructs consisting of collagen and PCL that are enhanced with nitric oxide-releasing nanoparticles can effectively prevent platelet adhesion while maintaining necessary burst pressures for vascular applications [Parenteau-Bareil et al., 2010].
Immune modulation
To combat foreign body responses, which compromise tissue function over time, strategies that incorporate zwitterionic surface grafting on alginate beads have demonstrated promising results, significantly reducing fibrotic encapsulation. In combination, local dexamethasone release can curb pro-inflammatory cytokines while promoting the ingrowth of new tissue [Kohane & Langer, 2008].
Additionally, smart hydrogels that stiffen under strain can direct macrophage behavior toward reparative phenotypes, thereby improving local vascularization [Khan & Tanaka 2017].
Outlook
The future of biomaterials in tissue engineering lies in bridging the gaps between mechanical stability, vascular perfusion, and immune tolerance. This holistic approach is beginning to shift the focus from structural simplicity to synergistic interactions that promote regenerative healing—resulting in advanced implants that not only integrate but actively orchestrate the healing response [Kohane & Langer, 2008], [Parenteau-Bareil et al., 2010].